Introduction
Blood glucose too high
Blood glucose too low
Diabetes
Diabetes healthcare and outlook
Introduction
The liver and the pancreas have a central role in the regulation of blood glucose concentration. The cells in the pancreas secrete the hormones which tell cells to take up glucose from the blood or not take it up. On demand, glucose is made from broken down glycogen in the liver.
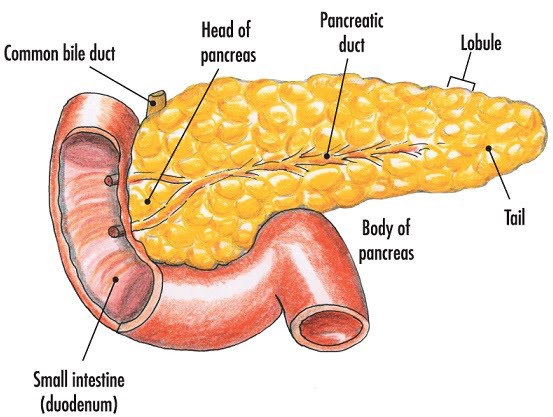
The pancreas has alpha and beta cells. Alpha cells secrete glucagon which increases blood glucose concentration, while beta cells secrete insulin which decreases blood glucose concentration. People with type 1 diabetes have destroyed beta cells, so their lack of insulin makes them have to take it via injections.
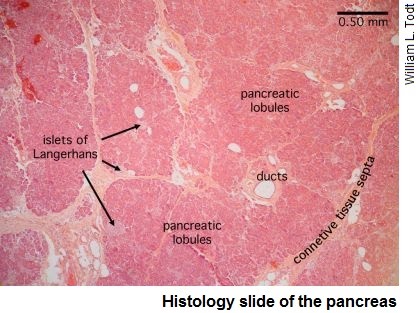
The islets of Langerhans contain the hormone-secreting endocrine cells including the alpha and beta cells. Most of them are the insulin-producing beta cells, with a smaller proportion of alpha cells.
Blood glucose is too high
The pancreas detects this, so it secretes insulin. This stimulates the uptake of glucose from the blood by cells, and the storage of it in the liver once it’s converted to glycogen. This reaction is called glycogenesis. The stages are:
- Insulin attaches to receptors on target cells
- This triggers a change in how many channel proteins are included in the cell membrane
- Separately, it also stimulates the activation of enzymes involved in converting glucose into glycogen….
