Vaccination
Antibiotics
Vaccination
Vaccinations prevent symptoms of an illness (such as flu or rubella) from developing, by creating a primary immune response to an unharmful substance that the body identifies as a pathogen. This could be an antigen, or the pathogen itself – dead or otherwise modified to prevent disease. Some vaccines are really successful and have prevented many diseases so far, yet the flu vaccine remains a challenge due to the above points. The virus changes its antigens, and there is great variation to start off with.
Booster vaccination is administered (e.g. every 10 years for tetanus) to make up for decreasing immunity over time due to memory cells dying. It boosts the immune response back to levels that confer protection against the disease.
Our natural immunity does not cover certain pathogens such as the flu virus. Vaccination attempts to induce artificial immunity which is an add-on to our natural immunity, by adding an artificially triggered response specific to a new pathogen that we did not have innately.
In the case of rabies, a vaccine is given containing antibodies in order to act as an emergency, passive treatment. Normally, the rabies vaccine would be given preventively to avoid getting the disease, but if someone is likely to have already got infected without prior vaccination, the administration of ready antibodies into their blood can help tackle the illness in its tracks. The antibodies would be obtained from someone else’s blood who has already raised an immune response to the pathogen. The passive vaccine of antibodies means that the patient does not need to wait to raise their own immune response, because the antibodies that would need to be made are simply delivered themselves straight into their blood.
Immunisation attempts through vaccination have had varying degrees of success for different diseases. Smallpox is an example of eradication through vaccination, while flu is an example of management and prevention through vaccination, but not long term eradication.
There are ethical considerations surrounding vaccination. On the one hand, large scale vaccination can prevent escalation of epidemics via herd immunity. When more people are immune to a certain infectious agent, transmission from person to person becomes more difficult even when a small number of cases do occur.
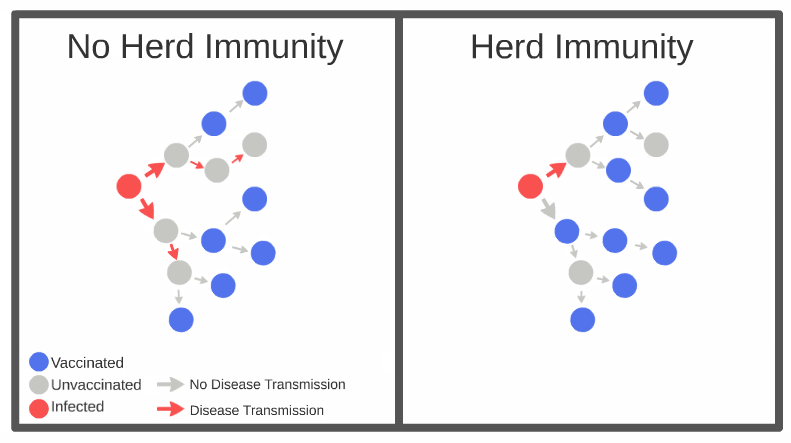
Therefore, anyone getting vaccinated would want to ensure others follow suit. On the other hand, the personal decision to get vaccinated can interfere with the goal of achieving a good immunity status for a given population against an illness. Some people would be cautious to get themselves or their children vaccinated due to suspected long term side effects.
The balance of personal autonomy versus achieving greater societal goals that require everyone to synchronise in their decision making has to be accomplished.
HPV vaccination
The Human Papilloma Virus (HPV) covers many different strains, some of which cause warts, and others which are associated with a higher risk of cervical cancer. The cervix is the lower part of the uterus. Mandatory vaccination is described by the NHS as “All girls aged 12 to 13 are offered HPV (human papilloma virus) vaccination as part of the NHS childhood vaccination programme.”….
